The CEO's Nighttime Peeing Problem: Why ‘No Water After 7PM’ Fails—A Case Study
Peeing at night is natural—the problem is staying wide awake after.
Yesterday, a CEO client said: "I've optimized everything—nutrition, training, biomarkers. But every night I wake up to pee and can't get back to sleep. I've tried everything. This one thing I can't solve is driving me crazy."
Melatonin, valerian, prescription aids, zero liquids before bed.
Nothing works.
Here's what I told him:
It's not just your bladder. It's your brain.
This conversation happens more often than you'd think.
Health-aware individuals who've dialed in every other aspect of their health but remain stuck on this one persistent issue.
The problem is that most approaches target the wrong systems.
Why Sleep Disruption Matters More Than You Think
When you wake up and can't get back to sleep, you're not just losing hours. You're fragmenting your sleep architecture in ways that compound over years.
The second half of the night contains the majority of your REM sleep—the phase responsible for memory consolidation, emotional regulation, and cellular repair processes that directly impact longevity. Losing this consistently doesn't just make you tired; it accelerates cognitive aging and increases inflammation markers that predict cardiovascular disease.
Individuals with fragmented sleep patterns have significantly higher levels of inflammatory cytokines like IL-6 and TNF-alpha, even when total sleep time appears adequate. Your body interprets frequent awakenings as stress signals, further disrupting the delicate hormonal cascade needed for deep sleep.
Therefore, solving nocturnal awakening isn't just about comfort—it's about preserving the biological processes that determine how well you age.
My Approach: Looking Beyond the Obvious
I used to wake up every night to pee too—and assumed that was the main issue.
Like most people, I tried the standard recommendations: no fluids after 7 PM, elevated legs, magnesium supplements, and every sleep hygiene protocol available.
However, I noticed the real problem wasn't the waking itself. It was that I couldn't fall back asleep. My mind would stay alert, and I'd lose that second half of the night. The frustration would build, creating a cycle where anxiety about not sleeping made sleep even more elusive.
My breakthrough came when I stopped focusing on preventing the wake-up and started investigating why I couldn't return to sleep.
I began tracking patterns: What time did I wake? How long to fall back asleep? What was different on nights when I could versus couldn't return to sleep quickly?
The data revealed something unexpected.
On nights when I fell back asleep easily, my body temperature remained stable, my heart rate variability stayed in range, and my breathing patterns suggested maintained parasympathetic dominance. On difficult nights, these markers all shifted toward sympathetic activation—essentially, my nervous system was switching into alert mode when it should have stayed in rest mode.
Now I still wake up and still need to pee—but I fall back asleep without effort.
The difference isn't in my bladder; it's in how my nervous system responds to the awakening.
Nocturnal Urination—Nocturia—isn’t always about fluid overload.
It's often a mismatch between:
your circadian clock and vasopressin, a hormone that concentrates urine while you sleep.
Vasopressin follows a circadian rhythm, with levels typically rising in the evening and peaking during the night. This hormone signals your kidneys to retain water and produce more concentrated urine, naturally reducing nighttime bathroom trips.
When vasopressin secretion is blunted or poorly timed, the bladder fills faster—even if you stopped drinking hours ago.
Several factors can disrupt vasopressin timing:
Light exposure after sunset interferes with melatonin production, which helps regulate vasopressin release
Inconsistent sleep schedules confuse your circadian clock, leading to mistimed hormone release
Chronic stress can suppress vasopressin production
Age-related changes naturally reduce vasopressin sensitivity and production
This explains why "stop drinking water before bed" only works if timing was the actual cause.
Fluid Restriction Is Not Always The Solution
Most people try fluid restriction, but if the core issue is disrupted vasopressin signaling, all that does is dehydrate you.
Same goes for sleep supplements—they sedate, but don't reset the system that controls nighttime urine volume.
Furthermore, here's what most people miss: Waking once at night isn't necessarily disruptive—unless you can't fall back asleep. In those cases, the issue often isn't bladder volume.
It's a failure to reinitiate the parasympathetic cascade that governs deep sleep.
When you wake up, your body should naturally maintain what sleep researchers call "sleep inertia"—a state where your nervous system remains primed for sleep despite brief consciousness. If you fall back asleep easily and wake rested, your body may be adapting just fine to its natural rhythm.
The problem arises when the awakening triggers a full sympathetic nervous system response.
This could point to several underlying issues:
Overactivation of your alertness system at night - often related to insufficient GABA activity or stress hormone imbalance
Incomplete sleep pressure buildup - suggesting issues with adenosine clearance or circadian timing
Dysregulated body temperature - preventing the natural temperature drop needed for sleep maintenance
Also worth noting: melatonin rarely helps here—especially at high doses.
Melatonin is a timing signal, not a depth-builder. It tells your body when to initiate sleep processes but doesn't strengthen them. When mistimed, it can interfere with your internal rhythm instead of supporting it.
If this pattern happens around the same time each night, it's worth looking beyond hydration—and asking what signal your body is really sending. Your circadian clock might be trying to communicate something about light exposure, stress levels, or metabolic timing that fluid restriction can't address.
Understanding these mechanisms shifts the entire approach from symptom management to system optimization. Instead of fighting your body's signals, you work with its natural patterns to restore the seamless sleep architecture that supports long-term health.
Most people attack sleep disruption from the wrong angle and spend years on surface fixes.
The systematic approach I use helps identify what's actually broken, not just what's most obvious.
Do You Want Deeper Help With Your Sleep Disruptions?
VAULT SLEEP O.S. is the first release in my personalized roadmap series, built for people who’ve already tried magnesium, blue light blockers, and textbook sleep hygiene.
It’s personalized—because it’s layered and triaged.
You’ll identify the type of sleep disruption, frequency, then move through the exact biological and behavioral checkpoints that apply to you—step by step—with tailored tools & workbooks for each stage—so you can restore deep, consistent sleep.
Warmly,
—Kat
References
Fu, K. (2025, June 6). The 3 forms of sleep disruption that shrink your brain—and how to tell if your sleep is actually protecting you from cortical atrophy, brain shrinkage and neurodegeneration. The Longevity Vault. https://thelongevityvault.com/performance-longevity/brain-shrinkage-sleep/
Fu, K. (2025, June 12). Melatonin for sleep: Why it often fails—and what to do instead to stay asleep to prevent brain aging, cognitive decline, and toxin buildup at night. The Longevity Vault. https://thelongevityvault.com/performance-longevity/melatonin-for-sleep/
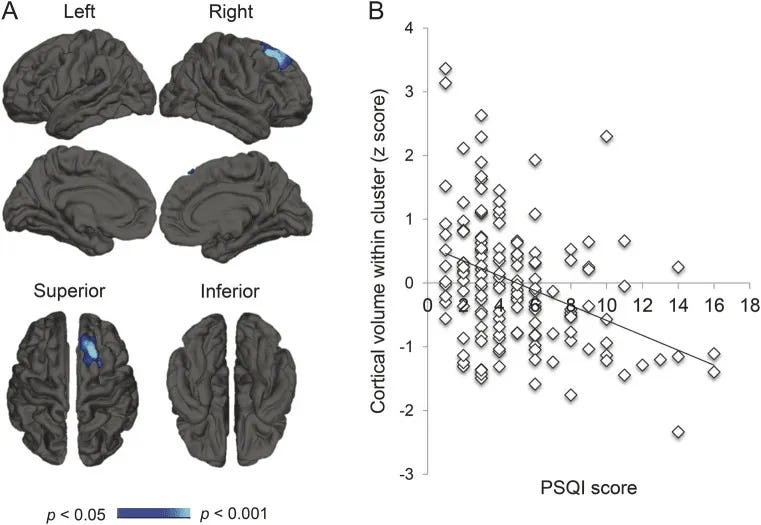
Cavaillès C, Dintica C, Habes M, Leng Y, Carnethon MR, Yaffe K. Association of Self-Reported Sleep Characteristics With Neuroimaging Markers of Brain Aging Years Later in Middle-Aged Adults. Neurology. 2024 Nov 26;103(10):e209988. doi: 10.1212/WNL.0000000000209988.
Kokošová V, Filip P, Kec D, Baláž M. Bidirectional Association Between Sleep and Brain Atrophy in Aging. Front Aging Neurosci. 2021 Dec 8;13:726662. doi: 10.3389/fnagi.2021.726662. PMID: 34955805; PMCID: PMC8693777.
Vidal-Pineiro, D., Parker, N., Shin, J. et al. Cellular correlates of cortical thinning throughout the lifespan. Sci Rep 10, 21803 (2020).
Sexton CE, Storsve AB, Walhovd KB, Johansen-Berg H, Fjell AM. Poor sleep quality is associated with increased cortical atrophy in community-dwelling adults. Neurology. 2014 Sep 9;83(11):967-73.
Lim AS, Fleischman DA, Dawe RJ, Yu L, Arfanakis K, Buchman AS, Bennett DA. Regional Neocortical Gray Matter Structure and Sleep Fragmentation in Older Adults. Sleep. 2016 Jan 1;39(1):227-35.