4 Hormone Misconceptions Keeping You From Fixing Your Sleep—At Any Age
I see hormone-related sleep disruption in men with declining testosterone, women during transitions & individuals in high-pressure lives.
Hormones & sleep are most often framed through the lens of menopause.
But in my work, I see hormone-related sleep disruption in many groups, including men with declining testosterone, women during reproductive transitions, adults in high-stress jobs, retirees, and those navigating major life changes.
The hormonal pathways differ, but the takeaway is the same: hormone-related sleep problems are not limited to one gender or one life stage.
Here are 4 common misconceptions about hormones & sleep that block clarity—and keep people searching for better sleep without results:
Misconception 1 (WHO): Hormones Only Affect Women in Menopause
The standard narrative focuses on estrogen drops during (peri) menopause.
That's true and important—but incomplete.
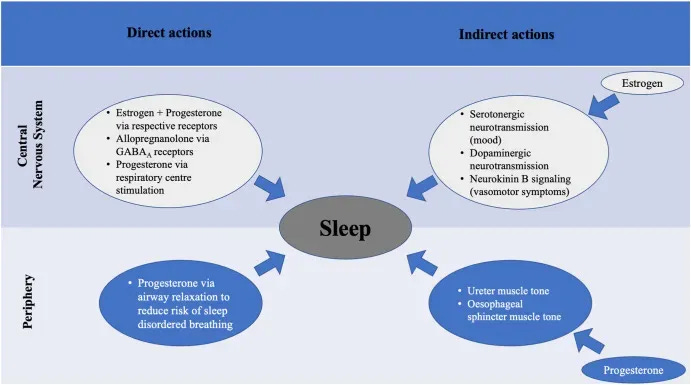
Estrogen is not the only hormone that matters for sleep.
Menopause is not the only time when hormones shift in ways that disrupt sleep.
And estrogen itself isn’t only a women’s hormone—men also produce and need it for normal physiology.
When estrogen balance changes in either sex, sleep architecture can be disrupted.
Recognizing this broader scope helps us see misconception #2…
Misconception 2 (WHAT): Hormone-Related Sleep Disruption Means Hormone Levels Are Too Low
Poor sleep rarely stems from one “low” hormone. Sleep depends on balance—ratios between hormones, timing across the 24-hour cycle, and how sensitive brain tissues are to those signals.
Both ends of the spectrum can create problems:
Estrogen: Higher levels can raise nighttime restlessness; lower levels can fragment sleep.
Progesterone: Lower levels reduce GABA’s calming effect; higher levels may push sedation into next-morning grogginess.
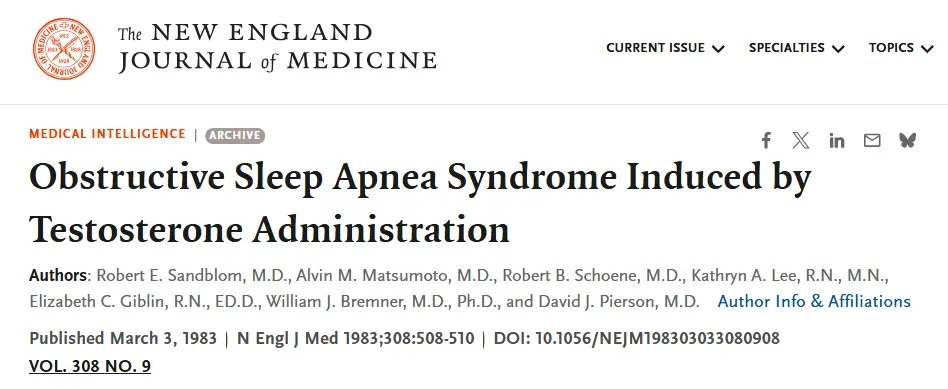
Testosterone: Lower levels affect deep sleep; higher levels can increase restlessness and worsen sleep apnea in susceptible men.
Hormones behave more like dimmer switches than on/off sleep toggles. The impact on sleep is therefore, rarely “more is better” or “less is worse.”
Raising a hormone which is ‘low’ may help—but without considering balance, it can just as easily create new problems.
This balance principle leads directly to the 3rd misconception: that certain hormones only matter for one gender.
If you want to learn how to map & support your own hormone–sleep patterns, subscribe to The Longevity Vault.
Each week I share strategies designed for individuals > 45 who want to sleep deeply, wake restored, and protect brain health for the decades ahead:
Misconception 3 (WHICH): Estrogen and Progesterone Are for Women, Testosterone Is for Men
Hormones aren’t confined to one gender. All adults carry and rely on all three: estrogen, progesterone, and testosterone.
Men produce estrogen and progesterone alongside testosterone.
Women produce testosterone alongside estrogen and progesterone.
The circulating amounts differ between sexes, but each gender depends on balance across all three for optimal sleep (& normal physiology).
When any one hormone becomes disproportionate—whether elevated or low—sleep architecture can shift in ways that fragment rest and reduce recovery.
This sets up the 4th misconception: that hormone disruption is just a matter of aging…
Misconception 4 (WHEN): Hormone-Related Sleep Problems Only Come With Aging
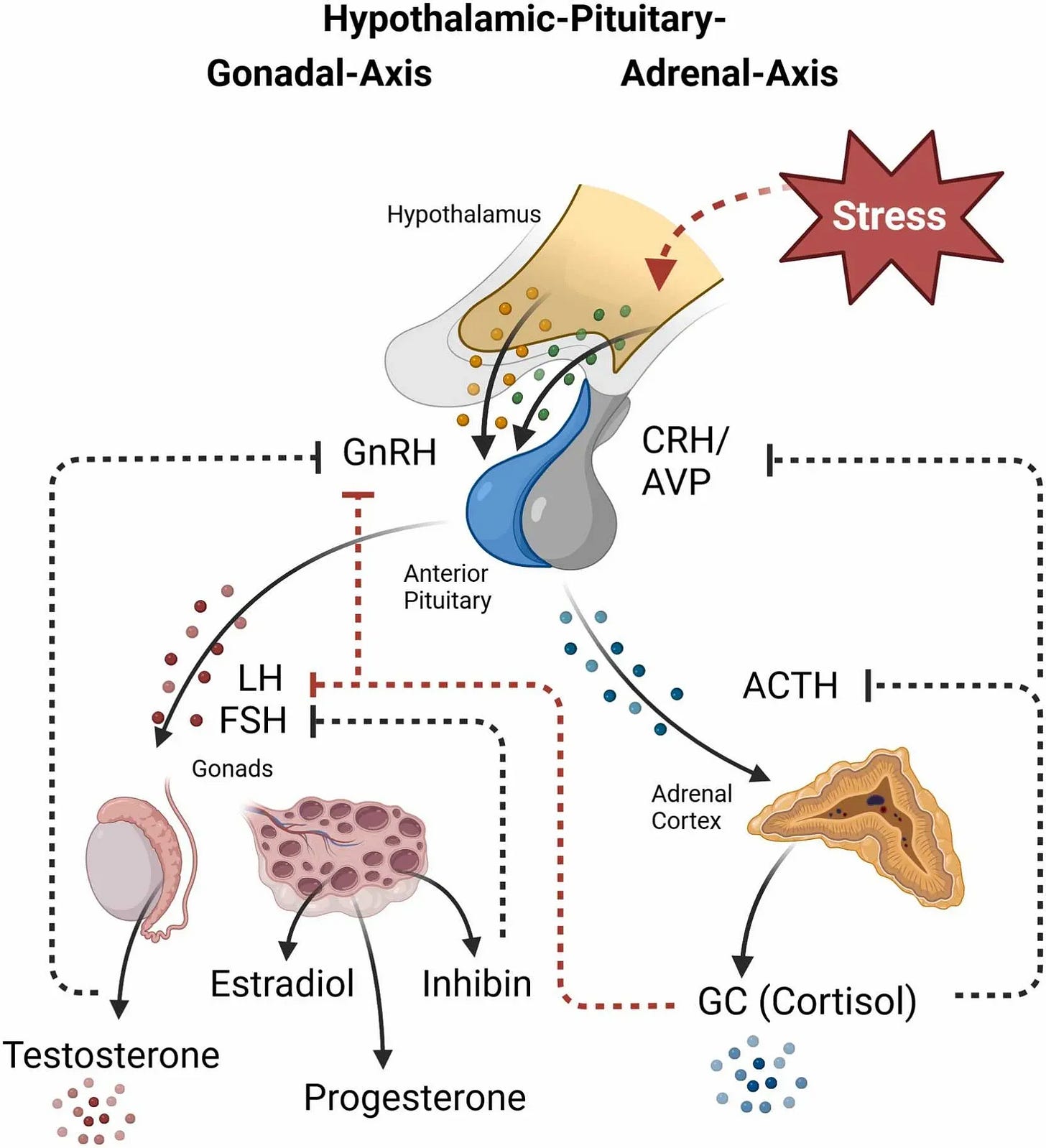
Yes, estrogen, progesterone, and testosterone decline with age.
But that’s only part of the picture.
Hormonal disruption can have multiple causes at every adult life stage:
Chronic stress affects multiple hormonal systems
Dietary shifts affect hormone synthesis
Environmental toxins disrupt endocrine function
Metabolic health changes influence hormone balance
Major life events create hormonal fluctuations independent of age
Medical conditions influence hormonal balance regardless of life stage
The takeaway is that hormone-related sleep disruption has many potential drivers, with aging being only one variable among many.
Moving Beyond the Misconceptions: What This Means for Your Sleep Recovery
These misconceptions have kept us confined to incomplete variables—age, gender, and single hormone levels—while missing the broader picture.
Here’s what changes now that we’ve clarified how hormones affect sleep:
Sleep challenges are seen less as demographic fate—and start looking like patterns you can influence
Hormone balance emerges as more important than absolute levels
Sleep disruption and hormone imbalance are recognized as mutually reinforcing—meaning you can improve one by addressing the other
The encouraging reality is this: hormone-related sleep disruption appears across all ages & both genders—but it also responds to systematic approaches that address underlying root causes rather than aiming for specific hormone levels.
And perhaps the most empowering realization of all: aging itself does not cause restless nights.
See you next time,
— Kat
P.S. If your sleep has changed since midlife—lighter, shorter, or more fragile under stress—habits alone are not enough. The midlife hormonal transition often shifts how your body builds and maintains NREM depth, but that function can be supported at any age.
Sleep OS: Hormones was designed for this stage. It offers a self-paced, step-by-step process to strengthen hormonal pathways that stabilize sleep—without hormone therapy or lab testing.
👉 You can learn more about my most popular program, the Trio Hormone Sleep Improvement Solution, here:
👉 Or, explore the foundational Sleep & Stress Sleep Solution here:
References
Haufe A, Leeners B. Sleep Disturbances Across a Woman's Lifespan: What Is the Role of Reproductive Hormones? J Endocr Soc. 2023 Mar 15;7(5):bvad036.
Morselli LL, Temple KA, Leproult R, Ehrmann DA, Van Cauter E, Mokhlesi B. Determinants of Slow-Wave Activity in Overweight and Obese Adults: Roles of Sex, Obstructive Sleep Apnea and Testosterone Levels. Front Endocrinol (Lausanne). 2018 Jul 12;9:377.
Sandblom RE, Matsumoto AM, Schoene RB, Lee KA, Giblin EC, Bremner WJ, Pierson DJ. Obstructive sleep apnea syndrome induced by testosterone administration. N Engl J Med. 1983 Mar 3;308(9):508-10.
Peter Y. Liu, Brendon Yee, Susan M. Wishart, Mark Jimenez, Dae Gun Jung, Ronald R. Grunstein, David J. Handelsman, The Short-Term Effects of High-Dose Testosterone on Sleep, Breathing, and Function in Older Men, The Journal of Clinical Endocrinology & Metabolism, Volume 88, Issue 8, 1 August 2003, Pages 3605–3613,
Wittert, Gary. The relationship between sleep disorders and testosterone in men. Asian Journal of Andrology 16(2):p 262-265, Mar–Apr 2014.
Sleep Foundation. (2025, July 16). The relationship between sleep and testosterone. Sleep Foundation
Lord C, Sekerovic Z, Carrier J. Sleep regulation and sex hormones exposure in men and women across adulthood. Pathol Biol (Paris). 2014 Oct;62(5):302-10. doi: 10.1016/j.patbio.2014.07.005. Epub 2014 Sep 11. PMID: 25218407.
McCosh RB, O'Bryne KT, Karsch FJ, Breen KM. Regulation of the gonadotropin-releasing hormone neuron during stress. J Neuroendocrinol. 2022 May;34(5):e13098.
van Broekhoven F, Bäckström T, van Luijtelaar G, Buitelaar JK, Smits P, Verkes RJ. Effects of allopregnanolone on sedation in men, and in women on oral contraceptives. Psychoneuroendocrinology. 2007 Jun;32(5):555-64.
Söderpalm AH, Lindsey S, Purdy RH, Hauger R, Wit de H. Administration of progesterone produces mild sedative-like effects in men and women. Psychoneuroendocrinology. 2004 Apr;29(3):339-54.
Verkes, R. & Broekhoven, F. & Smits, Paul & Buitelaar, Jan & Backstrom, Torbjorn. (2008). Sex differences in sedative effects of allopregnanolone; a first-in-men study. British Journal of Clinical Pharmacology - BRIT J CLIN PHARMACOL. 295-296.
Tančić-Gajić M, Vukčević M, Ivović M, Marina LV, Arizanović Z, Soldatović I, Stojanović M, Đogo A, Kendereški A, Vujović S. Obstructive Sleep Apnea Is Associated With Low Testosterone Levels in Severely Obese Men. Front Endocrinol (Lausanne). 2021 Jul 26;12:622496.
Barrett-Connor E, Dam TT, Stone K, Harrison SL, Redline S, Orwoll E; Osteoporotic Fractures in Men Study Group. The association of testosterone levels with overall sleep quality, sleep architecture, and sleep-disordered breathing. J Clin Endocrinol Metab. 2008 Jul;93(7):2602-9.
Domes G, Linnig K, von Dawans B. Gonads under stress: A systematic review and meta-analysis on the effects of acute psychosocial stress on gonadal steroids secretion in humans. Psychoneuroendocrinology. 2024 Jun;164:107004.
Liu, P.Y., Reddy, R.T. Sleep, testosterone and cortisol balance, and ageing men. Rev Endocr Metab Disord 23, 1323–1339 (2022).