The 2 Metabolic Systems Melatonin Disrupts—Even in Healthy Adults
Melatonin’s side effects aren’t limited to drowsiness or morning grogginess. Repeated or high doses may impair how your body handles glucose—even in healthy adults. Here’s what the studies reveal.
Why melatonin deserves its reputation—for the right reasons
Melatonin isn’t just a sleep molecule.
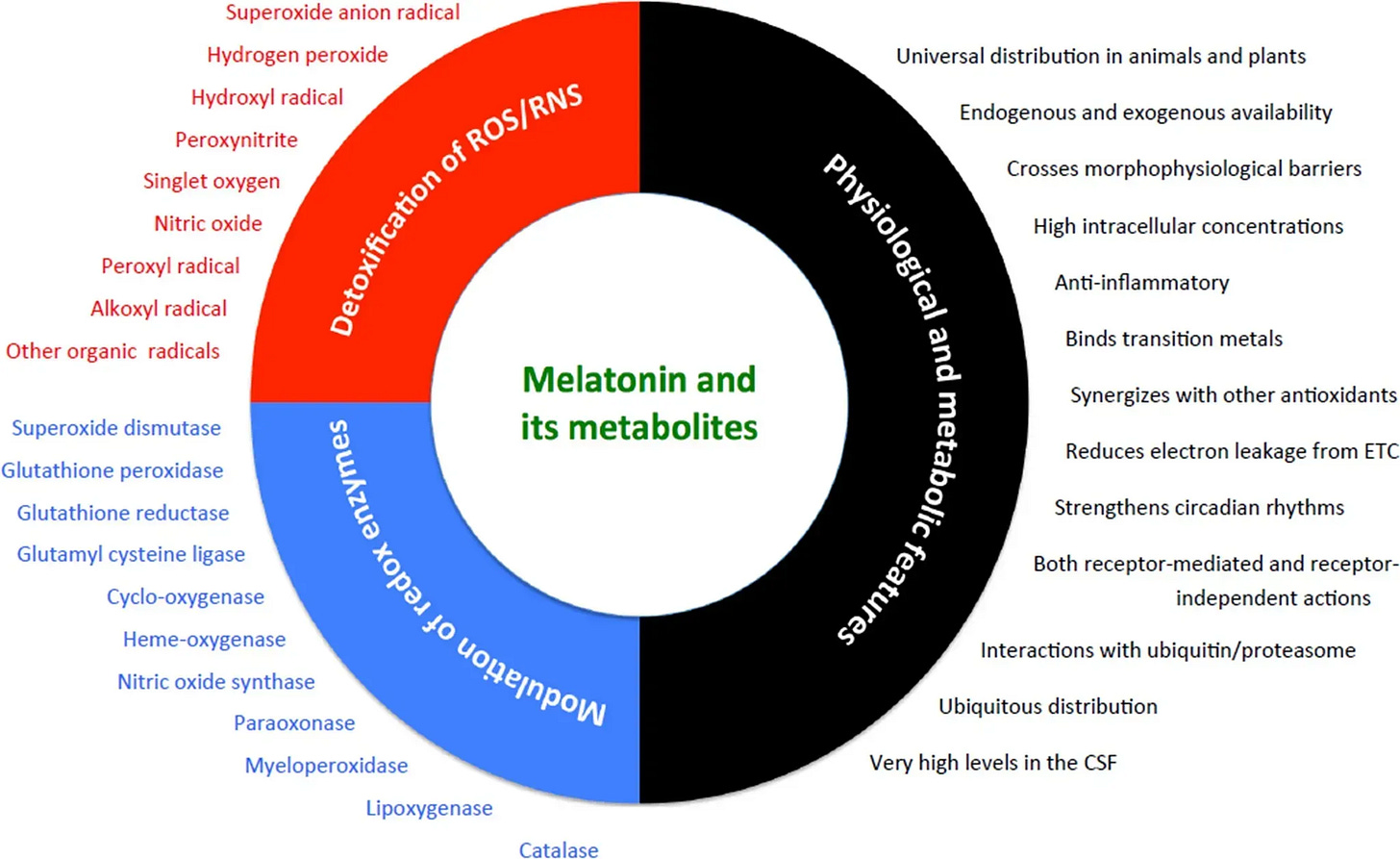
It’s one of the few compounds that concentrates inside mitochondria—the cell’s energy hubs and one of the body’s top sources of oxidative stress.
There, melatonin doesn’t just buffer damage—it helps prevent it. It directly neutralizes harmful radicals (like hydroxyl and nitric oxide species) while also upgrading the body’s own defense systems: enzymes like glutathione peroxidase and superoxide dismutase.
This is why melatonin has shown protective effects in the brain, heart, liver, and more. It’s also why it’s being studied for its potential in slowing age-related disease.
But here’s what many people miss:
It’s a hormone that acts on multiple tissues, not just your sleep-wake cycle.
But in this article, we’re focusing on one domain that gets far less attention:
How melatonin affects glucose regulation and metabolic health.
Can melatonin impair glucose metabolism—even if you're healthy?
Yes—and the mechanism is more nuanced than it first appears.
Melatonin receptors are expressed on pancreatic β-cells—the cells responsible for producing insulin. When activated at the wrong time, these receptors can blunt insulin release or impair downstream signaling.
In healthy individuals, this system works efficiently.
But when exogenous melatonin is introduced—especially at doses or times that don’t align with your body’s internal clock—it can override or mistime these pathways.
Would you like more content on melatonin or do you prefer other sleep topics?
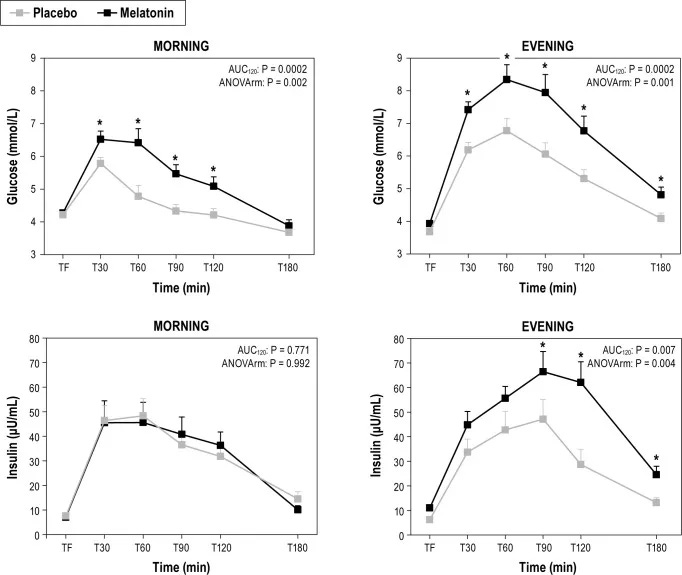
In a controlled trial involving 21 healthy adults (mean age 24, BMI ~23), researchers tested the metabolic impact of a 5 mg melatonin dose prior to a glucose challenge.
Here’s what they found:
A. When melatonin was taken in the morning, it reduced insulin secretion, leading to:
A 186% increase in glucose AUC
A 21% increase in peak glucose concentration
B. When taken in the evening, melatonin reduced insulin sensitivity, producing a
54% increase in glucose AUC compared to placebo
In both scenarios, glucose disposal was impaired. But the physiological driver differed.
This illustrates a central principle: melatonin’s effects on glucose metabolism are time-dependent and mechanistically distinct based on when the hormone is active relative to your circadian and feeding cycles.
Even in young, healthy adults—without obesity or prediabetes—these acute effects are measurable. Which raises a larger question:
What happens with chronic, mistimed use?
We don’t fully know.
But the short-term data suggest that evening melatonin use close to meals may chronically elevate postprandial glucose, subtly raising cardiometabolic risk over time.
What about people with metabolic conditions?
In metabolically compromised individuals, the effects aren’t just acute—they’re amplified.
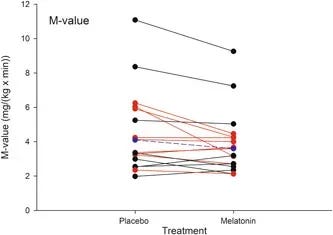
In a randomized, placebo-controlled crossover study, 17 men with type 2 diabetes were given 10 mg of melatonin nightly, 1 hour before sleep, for 3 months.
Outcomes were assessed using the gold-standard hyperinsulinemic-euglycemic clamp—a method that directly measures how much glucose is absorbed from the blood when insulin is artificially maintained at a constant level.
The results:
Insulin sensitivity dropped by 12% after melatonin treatment
Glucose-stimulated insulin secretion was reduced
The magnitude of effect varied by genotype—but the group-level outcome was still significant
This is important because melatonin doesn’t just act on insulin release; it can also affect how tissues like muscle and liver respond to insulin. In people who are already insulin resistant, this second-order disruption may compound metabolic inflexibility.
For patients with blood sugar dysregulation, mistimed melatonin isn’t a small variable—it may be the difference between stable fasting glucose and creeping hyperglycemia.
The authors of this study concluded that high-dose melatonin should be used cautiously in people with existing glucose dysregulation, given the potential for exacerbating insulin resistance.
And yet, melatonin remains one of the most casually used supplements in this group.
What should you do if you’re using melatonin—or thinking about it?
Melatonin isn’t inherently harmful.
But its effects are not one-size-fits-all—and that’s exactly the problem.
Most people don’t know if melatonin is helping or hurting their sleep.
Even fewer know how to time it based on their biology.
And almost no one is tracking when to take melatonin—some people need it 1 hour before bed, others respond best 3 to 4 hours earlier, depending on their circadian phase
That’s why Sleep OS exists—not as a single pill, but as part of the Longevity Vault Roadmap OS.
Sleep OS is a modular system inside the Roadmap that helps you:
Identify what’s actually disrupting your sleep (melatonin is just one signal we decode)
Learn how and when to use melatonin, if you can indeed benefit from it
Figure out what’s actually disrupting your sleep—even if you’ve already dialed in magnesium, caffeine, light, cold room, etc.
Sleep OS helps you uncover and correct the other factors still disrupting your rhythm—even when melatonin isn’t the issue.
If you’ve ever wondered:
“Why do I feel groggy after melatonin?”
or “Why does it sometimes work… and sometimes not?”
This is where you’ll find answers that match your physiology—not someone else’s.
📫 Want to be notified when Sleep OS opens?
References
Lauritzen ES, Kampmann U, Pedersen MGB, Christensen LL, Jessen N, Møller N, Støy J. Three months of melatonin treatment reduces insulin sensitivity in patients with type 2 diabetes-A randomized placebo-controlled crossover trial. J Pineal Res. 2022 Aug;73(1):e12809. doi: 10.1111/jpi.12809. Epub 2022 Jun 9. PMID: 35619221; PMCID: PMC9540532.
Rubio-Sastre P, Scheer FA, Gómez-Abellán P, Madrid JA, Garaulet M. Acute melatonin administration in humans impairs glucose tolerance in both the morning and evening. Sleep. 2014 Oct 1;37(10):1715-9. doi: 10.5665/sleep.4088. PMID: 25197811; PMCID: PMC4173928.
Reiter, R.J.; Sharma, R.; Chuffa, L.G.d.A.; Simko, F.; Dominguez-Rodriguez, A. Mitochondrial Melatonin: Beneficial Effects in Protecting against Heart Failure. Life 2024, 14, 88. https://doi.org/10.3390/life14010088
Sletten TL, Vincenzi S, Redman JR, Lockley SW, Rajaratnam SM. Timing of sleep and its relationship with the endogenous melatonin rhythm. Front Neurol. 2010 Nov 1;1:137. doi: 10.3389/fneur.2010.00137. PMID: 21188265; PMCID: PMC3008942.
Baskett JJ, Broad JB, Wood PC, Duncan JR, Pledger MJ, English J, Arendt J. Does melatonin improve sleep in older people? A randomised crossover trial. Age Ageing. 2003 Mar;32(2):164-70. doi: 10.1093/ageing/32.2.164. PMID: 12615559.
Buscemi N, Vandermeer B, Pandya R, Hooton N, Tjosvold L, Hartling L, Baker G, Vohra S, Klassen T. Melatonin for Treatment of Sleep Disorders. Evidence Report/Technology Assessment No. 108. (Prepared by the University of Alberta Evidence-based Practice Center, under Contract No. 290-02-0023.) AHRQ Publication No. 05-E002-2. Rockville, MD: Agency for Healthcare Research and Quality. November 2004.
Marupuru S, Arku D, Campbell AM, Slack MK, Lee JK. Use of Melatonin and/on Ramelteon for the Treatment of Insomnia in Older Adults: A Systematic Review and Meta-Analysis. J Clin Med. 2022 Aug 31;11(17):5138. doi: 10.3390/jcm11175138. PMID: 36079069; PMCID: PMC9456584.
Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: melatonin for the treatment of primary sleep disorders. PLoS One. 2013 May 17;8(5):e63773. doi: 10.1371/journal.pone.0063773. PMID: 23691095; PMCID: PMC3656905.
Fu, K. (2025, June 6). The 3 forms of sleep disruption that shrink your brain—and how to tell if your sleep is actually protecting you from cortical atrophy, brain shrinkage and neurodegeneration. The Longevity Vault. https://thelongevityvault.com/performance-longevity/brain-shrinkage-sleep/
Fu, K. (2025, June 12). Melatonin for sleep: Why it often fails—and what to do instead to stay asleep to prevent brain aging, cognitive decline, and toxin buildup at night. The Longevity Vault. https://thelongevityvault.com/performance-longevity/melatonin-for-sleep/