The 3 Midlife Sleep Patterns Linked to Early Brain Aging
Why "normal" sleep struggles in mid-life may be accelerating cortical thinning, memory consolidation issues, and executive function decline—even if you're still getting 7+ hours a night.
Midlife sleep issues are often brushed off as routine stress or normal aging.
But new longitudinal MRI data suggests something else may be happening beneath the surface: brain volume loss tied to the quality—not just the quantity—of your sleep.
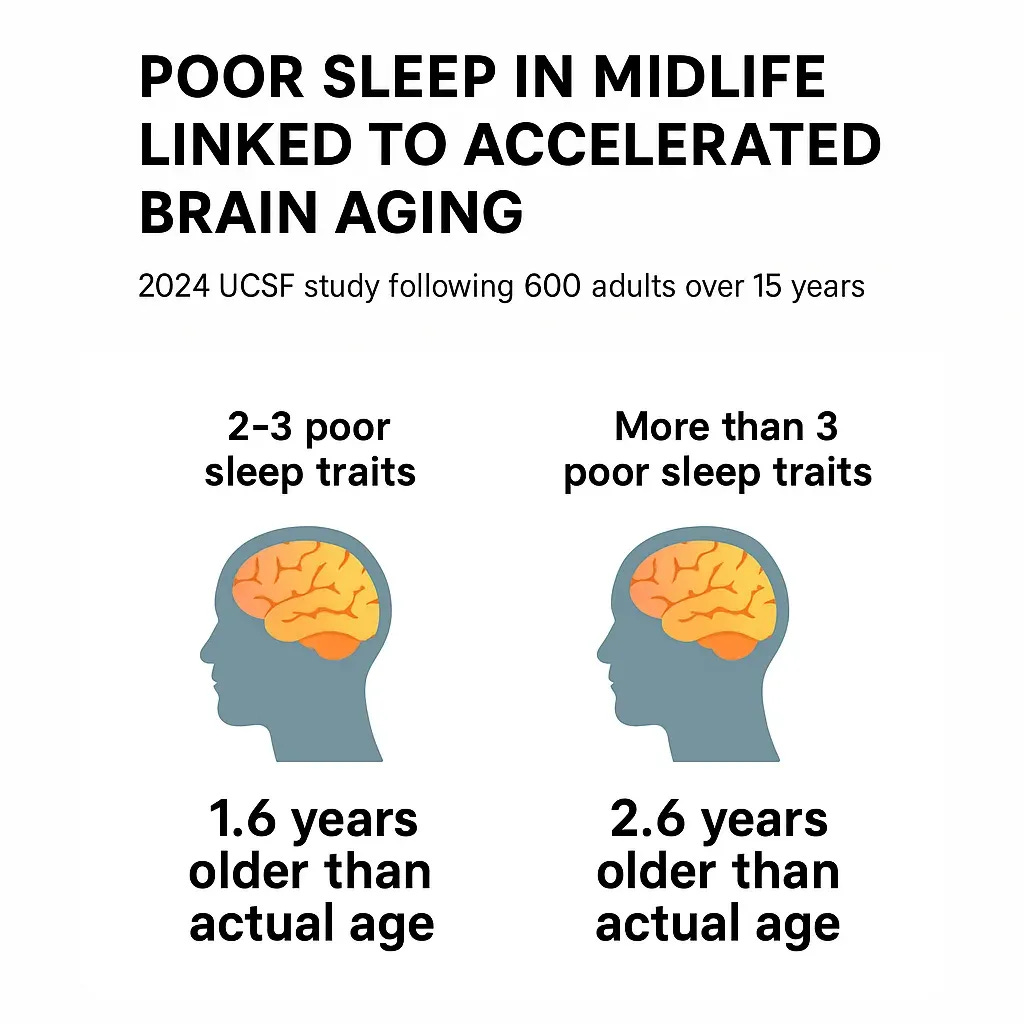
In a 15-year study published in 2024, UCSF researchers followed 589 adults (average age 40.4) and found that persistent midlife sleep disturbances predicted a structurally older brain in late midlife.
These weren’t isolated cases of sleep deprivation or clinical insomnia.
They were common patterns: difficulty falling asleep, waking too early, or sleep that felt consistently unrefreshing.
The Data: Brain Volume Loss Measured by MRI
The researchers used data from the CARDIA study, which included serial sleep assessments and structural brain MRI.
Participants were categorized based on the number of poor sleep characteristics (PSC) they reported—for example
poor sleep quality (SQ),
difficulty initiating or maintaining sleep (DIS, DMS),
early morning awakening (EMA), and
daytime sleepiness.
These characteristics were assessed at two time points, five years apart, to evaluate persistence.
15 years after baseline, participants underwent brain MRI.
Using machine learning trained on healthy aging patterns, the researchers estimated each person’s “brain age”—a composite marker derived from features like cortical thickness and volume in regions such as the hippocampus and prefrontal cortex.
The results were dose-dependent and statistically significant.
Adults with 2–3 poor sleep traits had brains that appeared 1.6 years older than their chronological age.
Those with > 3 poor traits showed an average 2.6-year brain age gap.
And the effect remained even after adjusting for potential confounders: physical activity, BMI, smoking, alcohol intake, hypertension, diabetes, cholesterol levels, and even total sleep time.
In short: it wasn’t just how long people slept. It was how well their sleep supported normal neurophysiological processes.
What That Brain Age Gap Really Means
Advanced “brain age” in this context reflects the type of structural deterioration that, over time, can precede cognitive decline. Cortical thinning, especially in the prefrontal cortex, affects executive function and emotional regulation. Brain volume loss in the hippocampus can erode memory consolidation before symptoms would meet clinical thresholds.
In this study, poor midlife sleep emerged as a stand-alone signal—associated with earlier onset of those very changes. And when poor sleep persisted across both midlife assessments, the associations with advanced brain age were even stronger.
As study author Dr. Clémence Cavaillès noted:
“Even if the cause of dementia is unrelated to sleep, poor sleep may advance or exacerbate cognitive symptoms.”
This underscores an important shift in how we view common midlife sleep problems. They may not simply reflect stress or lifestyle—but rather early dysregulation of systems like circadian timing, HPA-axis activity, and synaptic recovery.
So What Are The 3 Midlife Sleep Patterns That You Want To Watch For?
If your sleep feels fractured—even if you're still logging enough hours—it may be worth paying closer attention.
Especially if you're experiencing: