The first question I ask every client about their sleep
It’s not hours, deep sleep minutes, REM %, or your sleep score
“The first question I ask every client about their sleep isn’t ‘How many hours?’—it’s whether they wake up feeling restored.”
The most under-emphasized sleep metric isn’t a sleep score, REM %, or hours in deep sleep.
It’s this: restful sleep.
Because many of the most meaningful downstream consequences of poor sleep don’t show up as a bad sleep score. They show up like this: a mid-afternoon energy crash, brain fog, post-meal heaviness, and a growing requirement to nap just to function.
Those patterns matter because they indicate the body didn’t complete overnight recovery.
When restoration fails, the next day is often spent compensating—via stress hormones, stimulants, “pushing through,”—rather than a stable baseline.
That sets up the longevity question: if waking up unrested reflects incomplete recovery, does it also affect with biological aging?
Is restful sleep important for slowing down aging or aging better
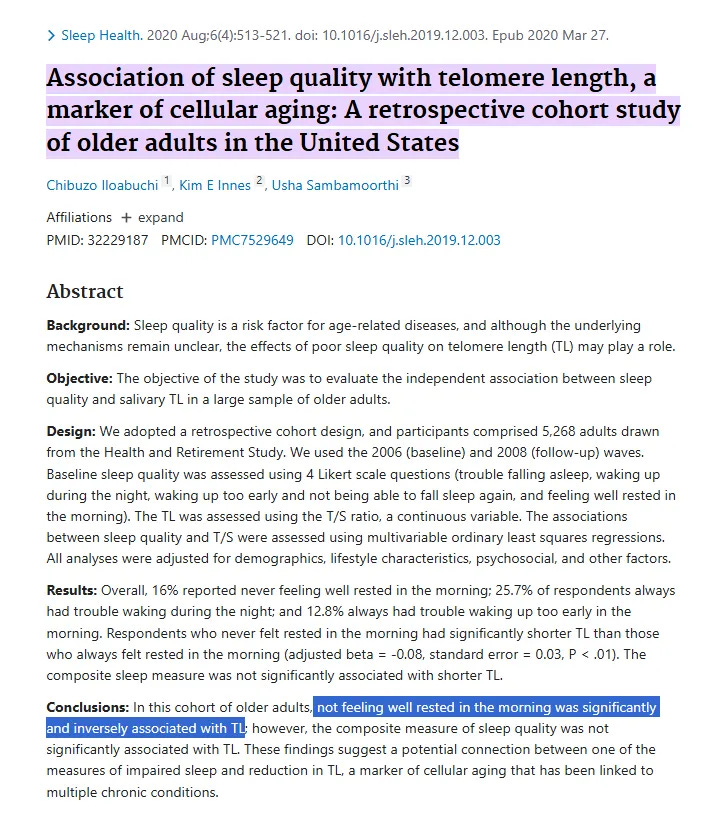
A large U.S. analysis involved 5,268 adults age 50+ from the Health and Retirement Study.
Sleep was assessed using 4 items:
trouble falling asleep,
waking during the night,
waking too early and not being able to fall back asleep, and
how often participants felt well rested in the morning.
The finding:
people who rarely/never felt rested in the morning had ~a 6% lower telomere-length compared to the average
(specifically, the difference was ~0.08 lower T/S. Relative to the cohort’s average T/S (~1.37))
Importantly, this association held even after adjusting for an extensive list of factors, including demographics (age, sex, race/ethnicity), socioeconomic status (education, income), health behaviors (physical activity, smoking), mood, body weight, and major chronic diseases.
In the same study, a composite sleep-quality score combining all four questions—including ‘feeling rested in the morning’—was not significantly associated with telomere length, while the single ‘rested’ item was.
So what is it about ‘restful sleep?’
“Feeling rested” = A ‘sleep outcome’—whether your sleep delivered recovery.
It can reflect sleep continuity, circadian alignment, overnight stress-hormone tone, and how often the brain gets pulled into lighter sleep by pain, or, relevant to most of you, midlife and advanced age hormonal changes that:
increase sympathetic activation and lower the arousal threshold—making sleep more easily disrupted
a higher likelihood of needing to pee at night
reduction of GABA tone
temperature instability (night sweats, overheating, in both men and women).
When recovery is repeatedly incomplete, the body runs with higher background stress and immune activation the next day, which maps onto mechanisms linked to cellular aging (including telomere dynamics).
Actionable Step: Treat “I don’t wake up restored” as a root-cause problem
From there, the next step is to revisit the factors that disrupt restful sleep.
Here are some practical steps that can help address unrestful sleep in midlife and advanced age.
I am sure many of you will have considered them before, seeing them together may help you notice which still need attention right now.
Rule out high-impact causes that rise with age: sleep apnea risk, pain/inflammation, and medication.
Anchor your circadian system: consistent wake time, strong morning light, and earlier movement.
Use naps strategically: earlier and shorter when needed (a booster)
Treat a daily irresistible nap as a signal that nighttime restoration is not completing.
Reduce fragmentation: limit late caffeine/alcohol
Track a daily “rested on waking” score including next-day recovery markers (brain fog, energy steadiness, post-meal crash intensity, afternoon crash, and nap requirement), not just time in bed or wakups.
Even though inadequate sleep can have wide-ranging impacts, those impacts aren’t permanent. With a clear understanding of what’s disrupting your sleep, targeted fixes can make restoration and long-term repair much more achievable.
P.S. If you recognize yourself in this pattern—midlife or advanced age, generally health-conscious, but still not waking rested—that’s who Sleep OS: Hormones is built for.
Sleep OS: Hormones helps you work on that baseline directly—without sleep medications, without more supplements, and without costly hormone workups—so you can reestablish full-night sleep and reduce the pressure sleep loss puts on brain aging and dementia risk.
👉 You can learn more about my most popular program, the Trio Hormone Sleep Recovery Course, here:
Get Trio Hormone Sleep Solution →
👉 Or, explore the foundational Sleep & Stress Single Hormone Sleep Recovery Course, here:
Get Sleep & Stress Single Hormone Solution →
A recent Sleep OS member described it this way:
‘I still get up once to use the bathroom, but I fall back asleep in seconds and I’m actually satisfied with my sleep again.
References
Iloabuchi C, Innes KE, Sambamoorthi U. Association of sleep quality with telomere length, a marker of cellular aging: A retrospective cohort study of older adults in the United States. Sleep Health. 2020 Aug;6(4):513-521. doi: 10.1016/j.sleh.2019.12.003. Epub 2020 Mar 27. PMID: 32229187; PMCID: PMC7529649.