The CEO's Nighttime Peeing Problem—A Case Study
Why ‘No Water After 7PM’ Fails
Recently, a CEO client said: “I’ve optimized everything—nutrition, training, biomarkers. But every night I wake up to pee and can’t get back to sleep. I’ve tried everything. This one thing I can’t solve is driving me crazy.”
Melatonin, valerian, prescription aids, zero liquids after 7. Nothing worked.
Here’s what I told him: It’s not just your bladder. It’s your brain.
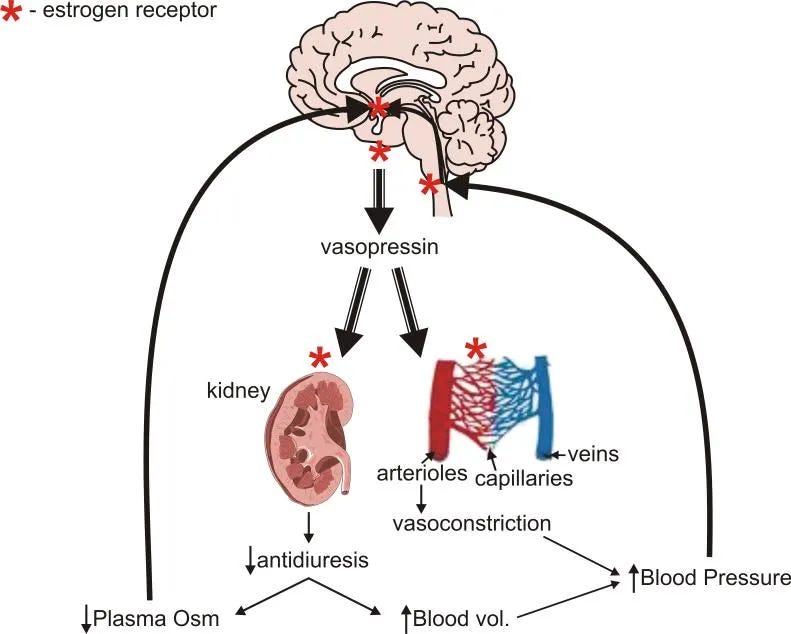
To understand what that means, we have to first look at our anti-diuretic hormone (ADH), also called vasopressin.
Waking Up To Pee vs. The Bladder
The Anti-Diuretic Hormone (ADH) is your body’s water-retention signal. It follows a circadian pattern: levels should rise at night so the kidneys concentrate urine and slow bladder filling.
In midlife, this nighttime fluid processing pattern often becomes unstable — and when it does, two things happen:
Light Sleep: Your sleep depth is more fragile, so your “wake threshold” is lower.
Altered ADH: Midlife reproductive-hormone shifts change how ADH behave meaning your kidneys process water differently at night.
Put together, that can sometimes appears as what I call the phantom urge:
You feel a need to pee every few hours, but when you go, you barely pass any urine—and then can’t get back to sleep. The problem isn’t an overactive bladder.
Because the sleep is light and unstable, the brain registers tiny signals from the bladder that a deeply asleep brain would ignore.
The urge didn’t pull you out of deep sleep. The lack of deep sleep allowed you to feel the urge + to prevent you from falling back asleep.
[Note: Here I’m focusing on functional and non-medical contributors. Sudden or major changes in urination frequency or volume should always be evaluated by a physician.]
The Solution: Solving the Sleep, Not the Bladder
I used to wake up every night to pee too—and assumed that was the main issue. Like most, I started with no fluids after 5/6/7 PM. I even tried no fluids after 3pm. None worked.
It was so disruptive I went to a urologist. Then a second, for another opinion. I did the full workup—bladder ultrasound and the flow-measurement chair—twice.
The result each time: “Everything is normal.”
The conclusion each time: “Too much water at night—stop drinking after 7 p.m.”
After 12 months of tests and 2 specialists, I was back where I started.
I found my solution when I stopped focusing on preventing the “need to pee” and started addressing why I had the phantom urge + why I couldn’t return to sleep.
Today, I still wake up and need to pee—every night—mostly because I genuinely feel better having (quite a bit of) liquids with dinner—but I fall back asleep without effort also, every night.
My bladder didn’t get bigger or become less active and I have fluids in the evening, often past 8 p.m. (plus, I really enjoy tea after dinner!).
The difference is that my sleep has become high quality, deeper, and more robust.
So in the rest of this article, we’ll look at three pieces:
why nighttime urination—nocturia—isn’t always about fluid overload,
why this pattern shows up so often in midlife, and
how I have helped others turn nighttime bathroom trips into non-events—and how you can achieve the same.
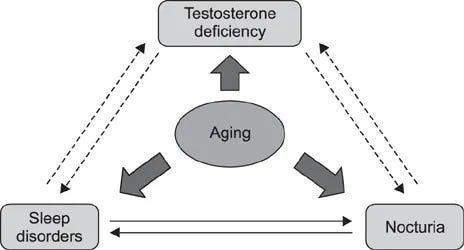
The Chain Reaction: Testosterone/Estrogen Changes → ADH → Bladder Signaling
The pattern many notice in midlife—lighter sleep, louder bladder signals, faster urine production—doesn’t begin with hydration. It begins with reproductive hormone changes:
Testosterone
Androgen (testosterone) receptors —where cells receive testosterone for it to act— exist in both the brain’s control center and kidney tissue. When testosterone function is impaired—not just low, but poorly utilized—two things happen simultaneously: more urine is produced at night, and the brain remains in a lighter, more arousable state.
Estrogen
Estrogen receptors —where cells receive estrogen for it to act—regulate ADH signaling and kidney behavior. When estrogen function is adequate—not just present, but properly received at the receptor—the body runs “night mode” on water: less urine, more concentrated, slower bladder filling. When function is impaired, sleep gets lighter and the system that concentrates urine at night becomes less efficient.
Progesterone
Progesterone supports deeper sleep and lowers nighttime arousal. When progesterone support weakens, sleep becomes shallower—and small bladder signals that a deeply-asleep brain would ignore now feel loud enough to wake you.
The net effect in midlife:
Even with normal water intake, the bladder fills at the wrong time and the sleep is too light for the brain to ignore it. This is why “stop drinking water before bed” doesn’t actually stop the 3am wakeups, nor does it improve your sleep.
That logic is reversed.
Instead, when you improve your sleep, you can drink water before bed and take bathroom trips without it impacting and how satisfied you are with your sleep.
One SleepOS member summed it up like this when I asked how well he was sleeping:
If you’re ready to stop treating the bladder and get a jump start—before the holidays—on the kind of hormone-stabilized sleep that protects your brain long term & lets you head into the season feeling good, this is the Trio Hormones Sleep Solution this member used: SleepOS Hormones Trio Hormone Sleep Solution
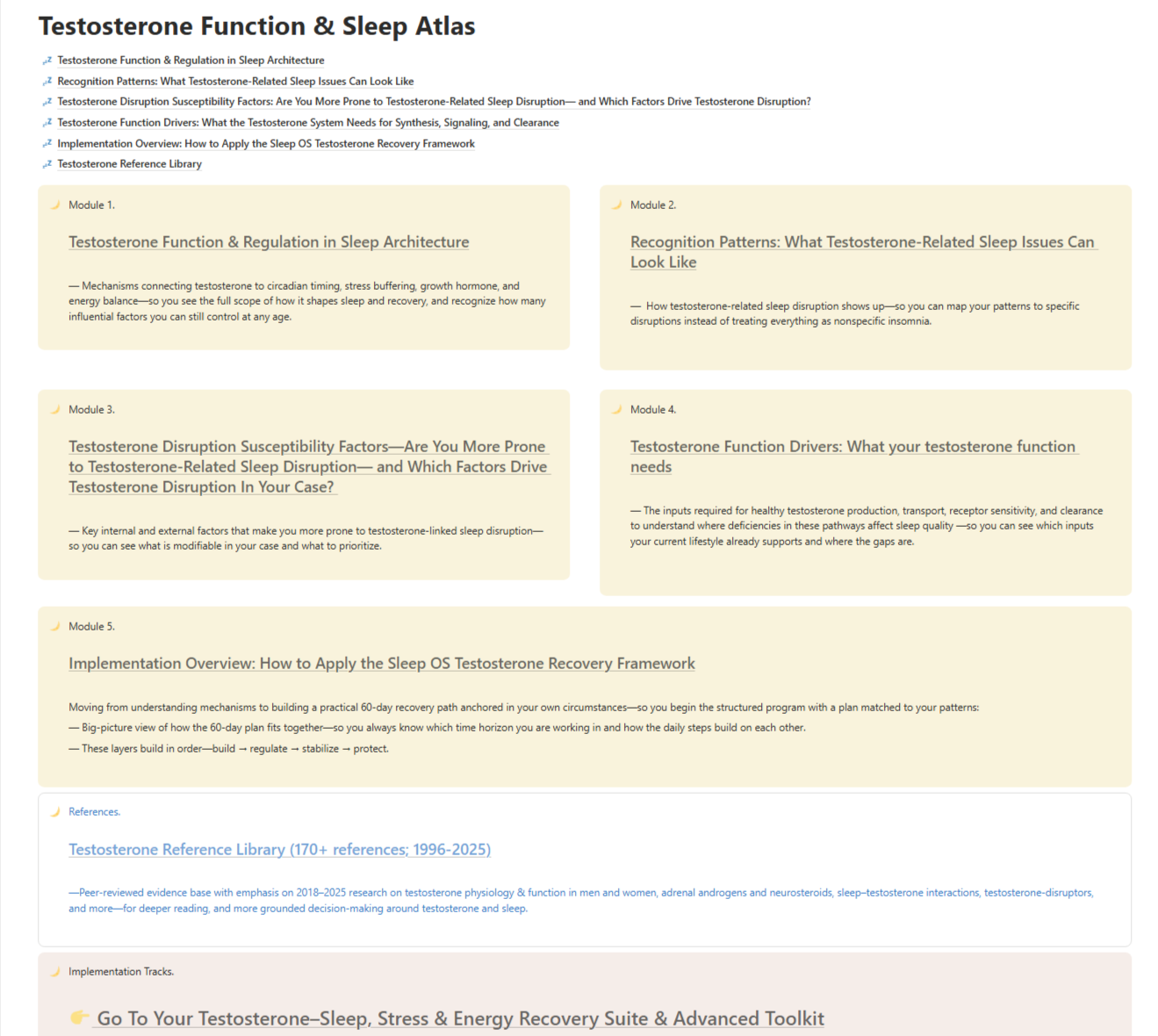
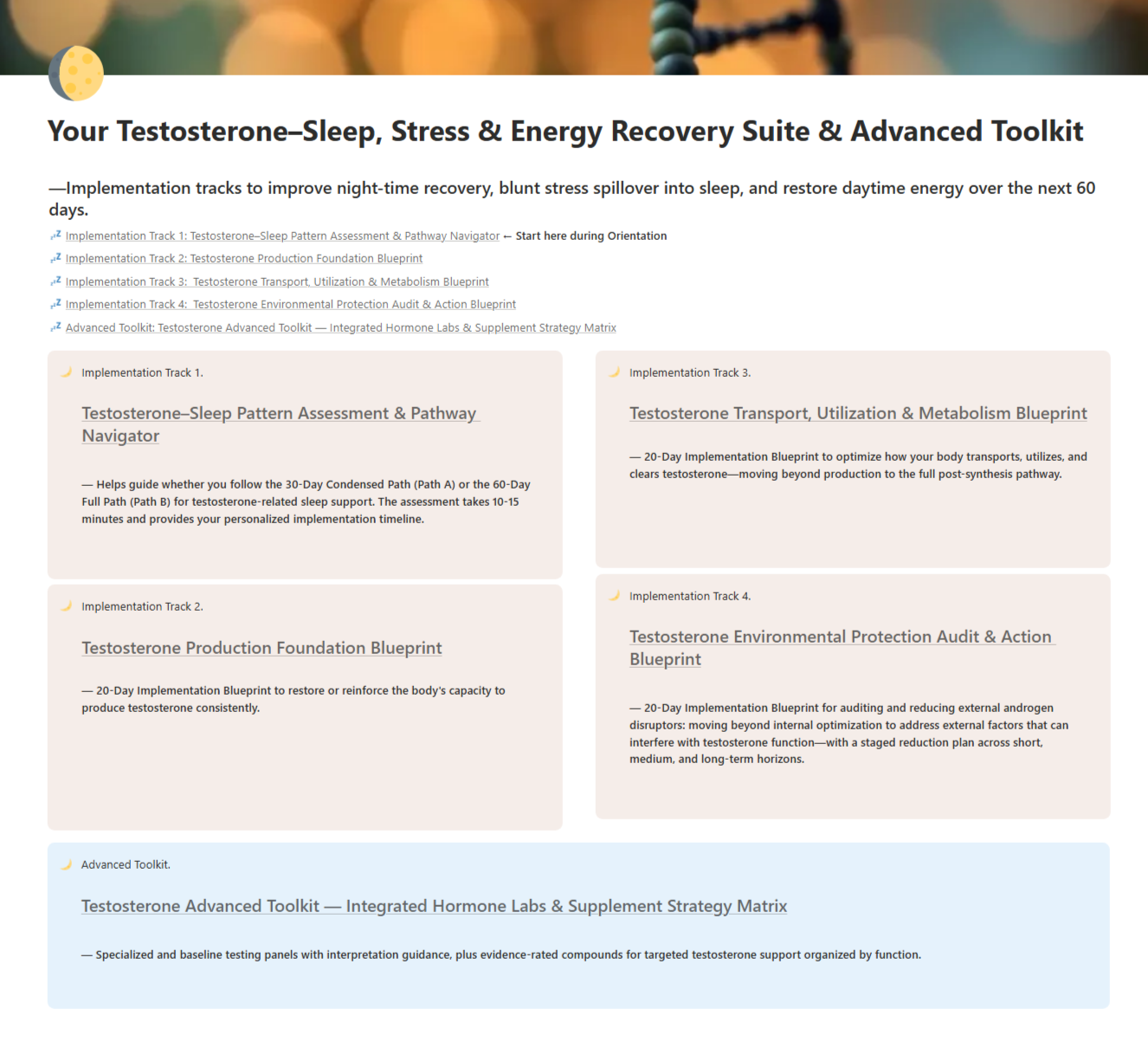
Here’s What You Get In Sleep OS – For Each Hormone (Testosterone as the Example)
How testosterone affects sleep architecture, who is most susceptible (10+ hormone disruption factors beyond age), and what your testosterone function needs across production, transport, hormone sensitivity, and clearance, synthesized from 170+ peer-reviewed studies.
Pattern recognition guide — how testosterone-related sleep disruption shows up
Your susceptibility profile — identify which factors are driving disruption in your specific case
60-day implementation sequence:
Days 1–20: Testosterone production support (step-by-step, 5 phases)
Days 21–40: Testosterone transport, hormone sensitivity, and clearance support (step-by-step, 5 phases)
Days 41-60: Hormone disruptors audit & guided plan to identify and reduce external disruptors of hormone function that work against testosterone regulation and sleep (step-by-step, 3 phase)
Bonuses included:
Starting Point Assessment & Planner — Map your pattern, coordinate your implementation (short path or long path), plan future maintenance
Integrated Hormone Diagnostics & Interpretation Suite — for when you want data: shows both standard and advanced tests you can run/request, where to get them, how to understand them, and what those multi-marker patterns mean for testosterone function and sleep (hormone testing is not just testing testosterone or estrogen levels)
Advanced Hormone Modulation & Supplement Strategy Matrix — evidence-rated supplement options organized by function (production, sensitivity, metabolism and clearance), with clear use-cases and safety considerations
👉 Start SleepOS Hormones Trio Hormone Sleep Solution Here
But, That’s you, Kat. My body is different.
You might be thinking, “Okay, that sounds nice, but I’ve been waking up at 3 a.m. for over a decade. My body just doesn’t do that.”
Fair.
Here’s what transformation looks like for someone else—same person, 3 months apart after working through Sleep OS Hormones:
Before Sleep OS (July): Here, this individual is getting 7 hours, but they perceive their sleep is not much better after trying the usual tips. The bladder signal wakes them up, and because the sleep depth is shallow, they stay awake.
After Sleep OS (October): Fast forward three months, his update looked very different. We didn’t shrink his liquid intake window or give him a bigger bladder.
But look at the result: “Back to sleep in seconds.”
This is the shift.
When you support the hormonal pathways—foundationally improving the Sleep Depth & Quality—the bathroom trip stops being a prolonged wake-up and becomes a non-event
You wake, you go, you return to bed, and your brain drops back into sleep almost immediately.
Here is another Sleep OS member (professional, mother, HRT user) describing that same state after Sleep OS Hormones:
That is the power of SleepOS Hormones.
Warmly,
Kat
P.S. If your sleep has changed since midlife—waking at 3 a.m., whether you need to pee or not, and then not falling back asleep—sleep hygiene is not enough. The midlife hormonal changes affects how your body regulates sleep and fluid processing, but that function can be supported at any age.
My digital program, Sleep OS: Hormones was designed for this. It offers a self-paced, step-by-step process to strengthen hormonal pathways that stabilize sleep—without supplements, prescriptions, hormone therapy or lab testing.
(1-3 extra ‘let’s keep an eye on it’ visits, a new wearable, and another round of supplements typically exceed the cost of Sleep OS: Hormones—and still don’t give you a coherent plan. This is meant to replace that scatter, not add to it)
👉 You can learn more about my most popular program, the Trio Hormone Sleep Improvement Solution here.
👉 Or, explore the foundational Sleep & Stress Single Hormone Sleep Improvement Solution here.
References
Pauwaert K, Goessaert AS, Robinson D, Cardozo L, Bower W, Calders P, Mariman A, Abrams P, Tubaro A, Dmochowski R, Weiss JP, Hervé F, Depypere H, Everaert K. Nocturia in Menopausal Women: The Link Between Two Common Problems of the Middle Age. Int Urogynecol J. 2024 May;35(5):935-946
Shigehara K, Izumi K, Mizokami A, Namiki M. Testosterone Deficiency and Nocturia: A Review. World J Mens Health. 2017 Apr;35(1):14-21.
Song QX, Suadicani SO, Negoro H, Jiang HH, Jabr R, Fry C, Xue W, Damaser MS. Disruption of circadian rhythm as a potential pathogenesis of nocturia. Nat Rev Urol. 2025 May;22(5):276-293.
Sladek CD, Somponpun SJ. Estrogen receptors: their roles in regulation of vasopressin release for maintenance of fluid and electrolyte homeostasis. Front Neuroendocrinol. 2008 Jan;29(1):114-27. doi: 10.1016/j.yfrne.2007.08.005.