Mouth taping has become the latest sleep optimization trend, with thousands of posts claiming it fixes everything from snoring to sleep quality.
The reality is more nuanced. While some people do experience benefits like reduced dry mouth and less partner disruption, a 2025 systematic review concludes that there is potentially "serious risk of harm for individuals indiscriminately practicing this trend."
More importantly, while mouth taping can address these specific sleep disruptions, it comes with safety risks and treats downstream symptoms while upstream causes remain unresolved.
The fundamental issue isn't that mouth taping never helps with sleep—it's that it addresses the symptom of mouth breathing without examining why your body defaults to this pattern in the first place.
For most people, the underlying reasons for mouth breathing represent better targets for sleep optimization with safer, more comprehensive benefits.
What's particularly concerning is how mouth taping gets positioned as a primary sleep optimization strategy when the limited research focuses on specific breathing disorders in clinical populations, not sleep improvement in healthy individuals seeking better rest.
What the Research Actually Shows About Sleep and Mouth Taping
The studies most frequently cited to support mouth taping examined surgical tape application in people diagnosed with mild sleep apnea—a medical condition where mouth breathing often compensates for compromised nasal airways. These trials measured specific clinical markers like apnea-hypopnea index (AHI) reduction, which indicates fewer breathing interruptions.
The most substantial data comes from controlled studies where participants underwent screening before tape application.
Researchers confirmed adequate nasal airway function through rhinomanometry testing and excluded candidates who couldn't tolerate the intervention during supervised trials. Under these highly controlled conditions, some studies documented reduced breathing events in sleep apnea patients.
However, the Rhee et al. systematic review, analyzing 10 studies with 213 patients, found mixed results even in these clinical populations.
While two studies showed statistically significant improvements in breathing disorder markers, others "offered no differences and even discussed potential risks." Critically, many studies excluded anyone with nasal obstruction—precisely the people most likely to mouth breathe and seek this intervention.
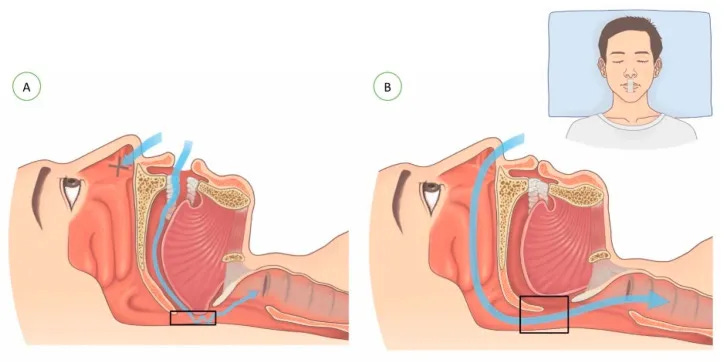
The mechanism explains both why mouth taping can improve sleep for some people and why it's problematic as a primary strategy.
Mouth breathing during sleep can cause frequent micro-arousals from dry mouth discomfort, throat irritation, and disrupted sleep continuity. When nasal breathing is adequate, eliminating mouth breathing can reduce these specific sleep disruptions.
However, mouth breathing often develops as a compensatory response to underlying issues: nasal congestion, structural airway problems, or breathing difficulties.
Taping addresses the mouth breathing symptom while leaving these root causes unresolved, creating potential safety concerns and missing opportunities for more comprehensive improvement.
My 3 Considerations for Sleep-Focused Mouth Taping
Rather than treating mouth taping as a general sleep optimization tool, I think about it as addressing a specific problem: residual mouth breathing after other factors have been ruled out.
Here are a few of the considerations that matter:
First: Are there signs of underlying breathing issues?
Waking up gasping, morning headaches, or persistent fatigue despite adequate sleep time suggest something more complex than simple mouth breathing habits. These symptoms indicate your breathing is already challenged during sleep, making mouth taping potentially counterproductive.
Second: Could this be a hydration or environment issue?
Before assuming structural problems, it's worth evaluating simpler explanations.
Are you adequately hydrated?
Sleeping in dry environments?
Taking medications that reduce saliva production?
Many cases of nighttime mouth breathing stem from dehydration or environmental factors that resolve with straightforward adjustments.
Third: Is this isolated dry mouth or part of a broader pattern?
If mouth breathing occurs alongside chronic nasal congestion, frequent sinus issues, loud snoring, or witnessed breathing pauses, these suggest structural airway problems that won't improve with tape alone. In these cases, addressing the underlying causes—deviated septum, allergies, or sleep-disordered breathing—makes more sense than symptom management.
When mouth taping does make sense, it's typically after ruling out these other factors and confirming that simple mouth breathing habits are the primary issue. Even then, it's addressing mouth dryness rather than fundamentally improving sleep architecture or addressing sleep disorders.
Why Mouth Taping Distracts from Real Sleep Improvement
The casual approach to mouth taping reflects a broader issue with how sleep optimization trends spread on social media. Complex physiological processes get reduced to simple interventions, often missing the underlying mechanisms that determine whether an intervention helps or hinders.
The false security aspect concerns me most.
When mouth taping reduces obvious symptoms like snoring or dry mouth, people often assume their sleep issues are resolved. However, if the underlying cause involves airway compromise, the breathing difficulties may persist while becoming less noticeable to partners. This can delay appropriate evaluation and treatment of legitimate sleep disorders.
There's also the anxiety factor.
For people with any sensitivity around breathing—whether from anxiety disorders or previous breathing difficulties—the sensation of restricted airflow can create sleep disruption that outweighs any potential benefits. The intervention designed to improve sleep quality ends up fragmenting sleep through heightened arousal and stress responses.
Perhaps most importantly,
the opportunity cost of focusing on mouth taping can delay addressing treatable root causes. Conditions like chronic sinusitis, nasal polyps, or structural abnormalities respond well to targeted treatment but may be overlooked if symptom management provides partial relief.
Mouth taping works best as a final optimization step for people who've already addressed underlying issues and confirmed normal nasal function. When used this way—addressing residual dry mouth after comprehensive evaluation—it serves its intended purpose rather than masking more significant problems.
The distinction matters: using mouth taping to manage confirmed mouth breathing habits after ruling out other causes versus using it as a first-line treatment for undiagnosed sleep or breathing issues represents fundamentally different approaches with very different risk profiles.
Have you tried mouth taping or noticed mouth breathing issues?
I'd love to hear what worked (or didn't) for you in the comments.
And if you want more of this root-cause approach to sleep, Sleep OS is my systematic framework for identifying and fixing the biological drivers behind sleep issues.
It's built for people who've tried the basics but need to go deeper than generic sleep advice.
References
Rhee J, Iansavitchene A, Mannala S, Graham ME, Rotenberg B. Breaking social media fads and uncovering the safety and efficacy of mouth taping in patients with mouth breathing, sleep disordered breathing, or obstructive sleep apnea: A systematic review. PLoS One. 2025 May 21;20(5):e0323643. doi: 10.1371/journal.pone.0323643. PMID: 40397877; PMCID: PMC12094774.
Zhang C, Shen Y, Liping F, Ma J, Wang GF. The role of dry mouth in screening sleep apnea. Postgrad Med J. 2021 May;97(1147):294-298. doi: 10.1136/postgradmedj-2020-137619. Epub 2020 Sep 10. PMID: 32913036.
Lee YC, Lu CT, Cheng WN, Li HY. The Impact of Mouth-Taping in Mouth-Breathers with Mild Obstructive Sleep Apnea: A Preliminary Study. Healthcare (Basel). 2022 Sep 13;10(9):1755. doi: 10.3390/healthcare10091755. PMID: 36141367; PMCID: PMC9498537.